Your PBM Profits From Complexity. You Pay for It.
Fiduciary pharmacy benefits administration that removes conflicts, simplifies the model, and holds us contractually accountable to employer outcomes.

Pharmacy Benefit Administration (PBA)
Claims adjudication, eligibility, plan configuration, prior authorization administration, and reporting with radical transparency. Employers, brokers, and TPAs gain control, predictability, and lower pharmacy spend while members get a smoother, more reliable experience.
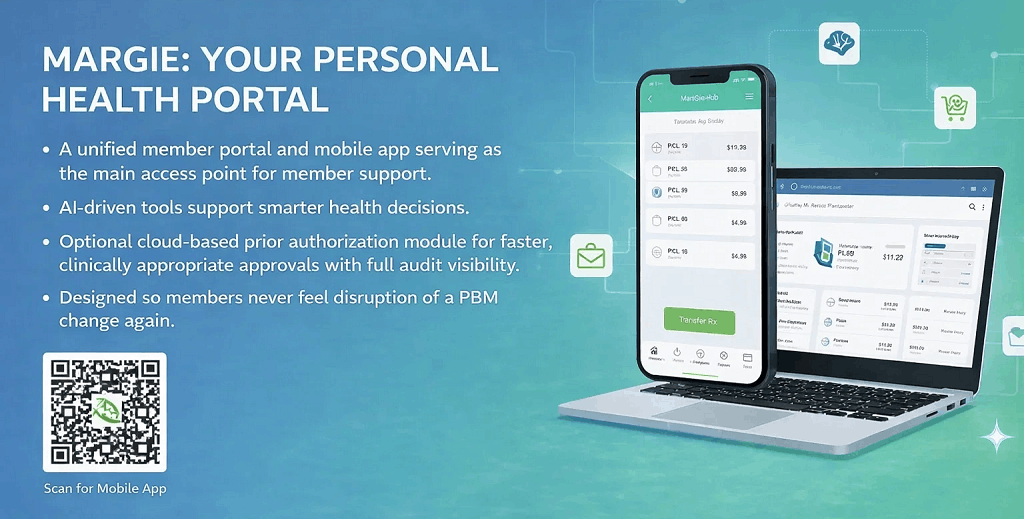
Member Portal and Mobile Application
A single member portal and mobile app built as the primary service layer. AI-driven tools support smarter decisions, optional built-in prior authorization reduces friction, and Mark Cuban Cost Plus Drugs is already integrated. Designed so members never feel the disruption of a PBM change again.
InsourceRx Analytics
Self-service dashboards for Rx and J-code claims. Built for finance, HR, and advisors. White-label and self-hosted options keep personally identifiable information and protected health information securely within your environment.
RxDC Reporting Software
RxDC reporting software captures, organizes, and submits required prescription drug cost data to meet federal transparency and compliance requirements. The key benefit is accurate, audit-ready reporting with less administrative burden, reducing compliance risk for plan sponsors.
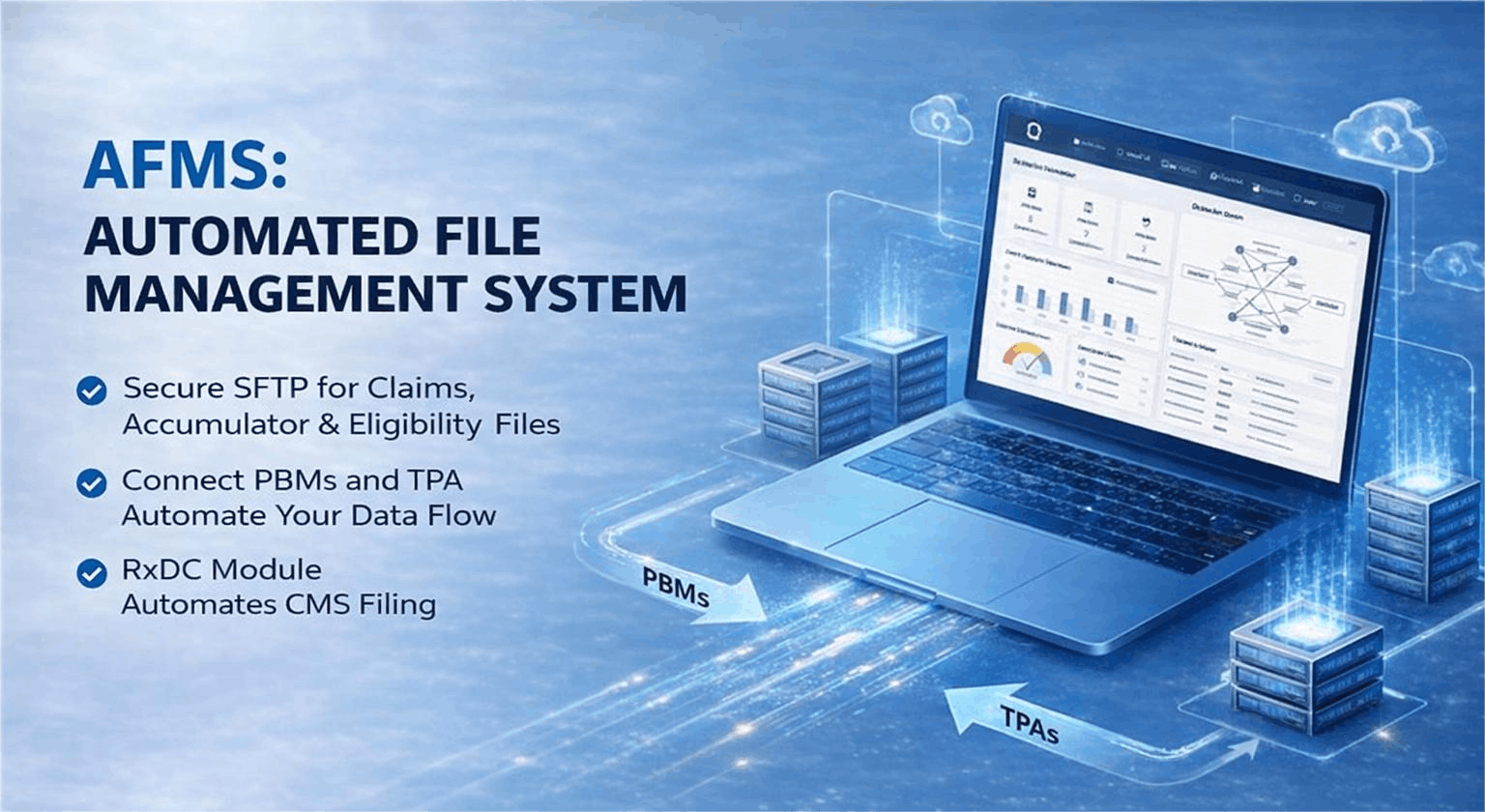
Automated File Management System (AFMS)
AFMS is an automated file management system that securely handles the intake, validation, and transfer of eligibility, claims, and accumulator files across PBMs, TPAs, and vendors with minimal manual effort. The key benefit is reduced operational risk and faster turnaround times by eliminating human error while maintaining a clear audit trail.
Specialty Drug Management
In-house specialty drug management program delivers hands-on oversight of high-cost specialty medications, including site of care control, utilization review, and sourcing decisions managed directly by our team. The key benefit is tighter cost control and faster intervention without relying on outside vendors, while protecting continuity of care for members.
Formulary and Utilization Management
Formulary and utilization management programs apply evidence-based coverage rules, prior authorization, and step therapy decisions managed directly by our clinical team. The key benefit is tighter cost control and faster decision-making without outside vendor influence, keeping pharmacy management aligned with a fiduciary standard of care.
Free Prescription Discount Card
Built for Fiduciaries
Every solution is purpose-built to uphold your fiduciary duty by minimizing conflicts of interest and protecting plan assets with radical transparency.
